OUR HER2 SOLUTION
What is HER2?
HER2 is a protein that promotes growth on the surface of all breast cells. Breast cancer cells with higher than normal levels of HER2 are termed either HER2-low or HER2-positive, as opposed to HER2-negative.
These HER2-positive cancers generally grow and spread faster but are much more likely to respond to treatments that target the HER2 protein. Until the end of 2022, only HER2-positive breast (and gastric) cancer patients were eligible to receive HER2- targeted treatment, with all other patients considered to be HER2-negative.
Recently, HER2 classification has been refined into three categories: HER2-positive, HER2-low and HER2-negative (or HER2-null), allowing more precise treatment approaches.
Treatment options
Treatment strategies are tailored according to the assessment of a patient’s HER2-status. Accurate classification of patients into the correct HER2 category (positive, low or null) is imperative to ensure the most suitable treatment regimen.
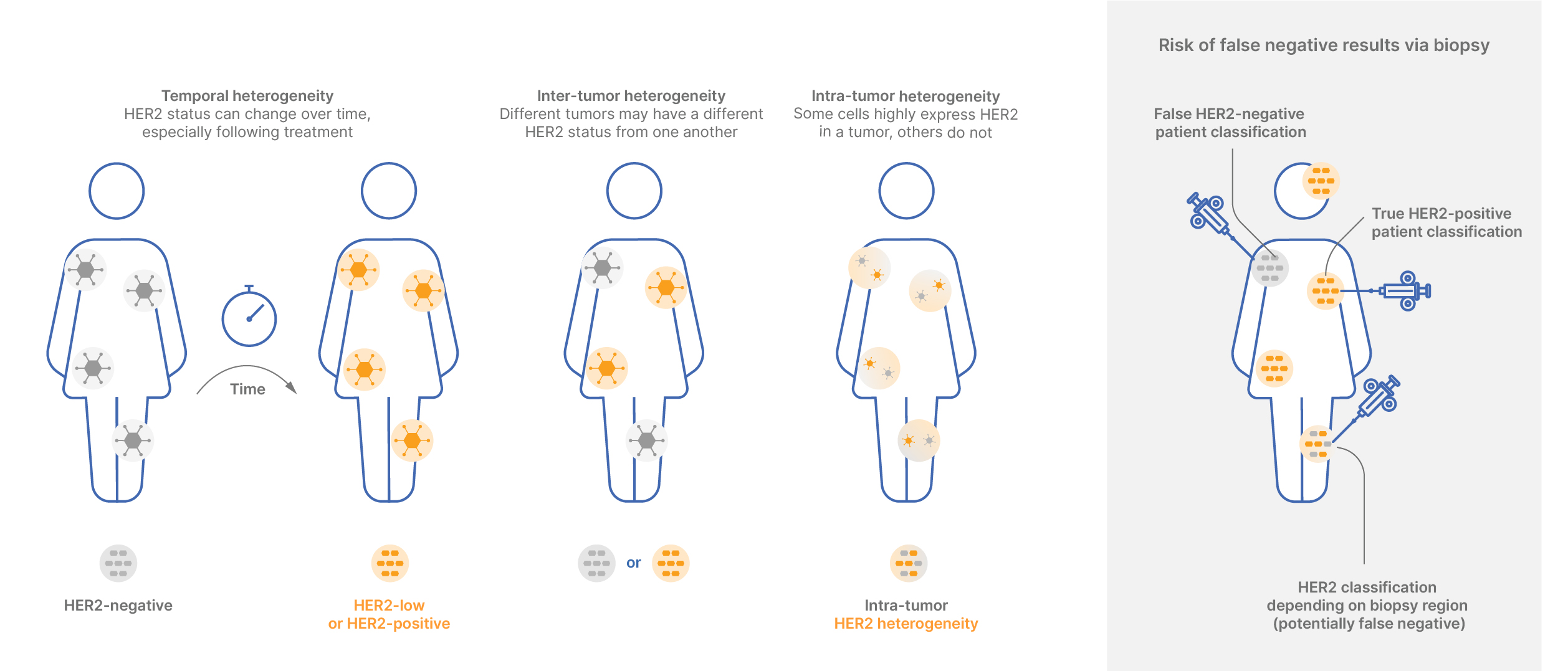
HER2 heterogeneity
The intricate nature of HER2 status is gaining recognition, as it frequently demonstrates variability within an individual patient and evolves over time. HER2 tumors can exhibit three type of heterogeneity: temporal, inter-tumor and/or intra-tumor.
Our technology plays a crucial role in facilitating informed decisions about biopsy localization, taking heterogeneity into account to ensure accurate diagnosis and treatment planning.
Technology impact on patient management
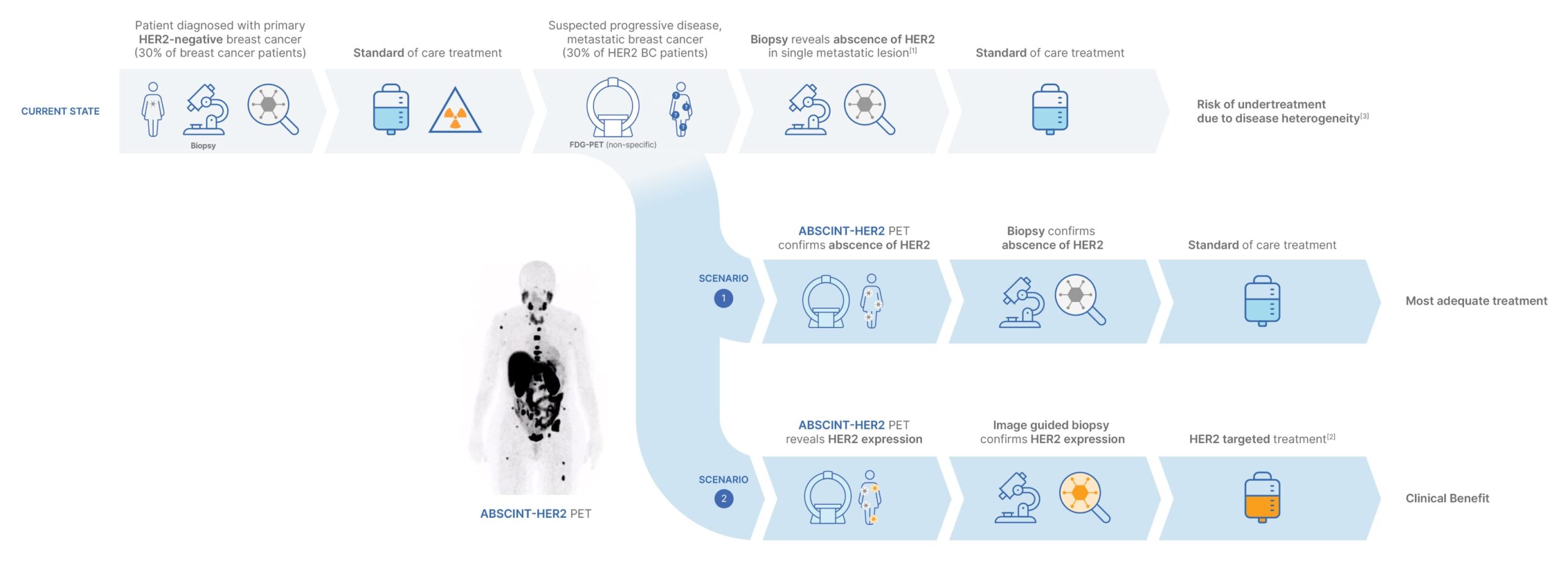
EXAMPLE 1:
Reclassification via image guided biopsy
The impact of our technology on patient management is profound, particularly in the context of re-evaluating HER2-status in breast cancer patients. For instance, patients initially diagnosed with HER2-negative breast cancer, who relapse with metastatic breast cancer, require a reassessment of their HER2-status.
Traditionally, this involves biopsying a lesion chosen at random, but this approach does not account for the possible variability and evolution of HER2-status across different lesions over time. ABSCINT’s HER2 PET tracer empowers clinicians to select the most appropriate lesion to biopsy for accurate status confirmation.
This image-guided biopsy can result in significant adjustments of the treatment regimen, offering substantial and tangible clinical benefits.
Reference:
[1] Biopsies (1-30 k€) may cause complications, are unable to pick up disease heterogeneity,and present up to 20% inaccurary
[2] e.g. Trastuzumab deruxtecan
[3] Holthuis EI, 2022 (Article)
EXAMPLE 2:
Patient follow-up
Patients diagnosed with HER2-positive cancer, despite receiving standard treatment, may encounter disease progression and metastases, potentially resulting in changes to the HER2 status of individual lesions.
In conjunction with broad and non-specific FDG-PET scans, the specificity of our HER2 tracer, ABSCINT-HER2, proves valuable for precise disease characterization, allowing assessment of HER2 tumor locations and heterogeneity, consequently guiding adapted cancer treatment.
The use of in vivo imaging, particularly in parallel with treatment, becomes indispensable for monitoring treatment response and HER2 status in individual lesions, enabling timely adaptations of therapeutic interventions to optimize patient outcomes.
The adapted treatment plan may include a combination of targeted therapies, chemotherapy, and possibly other emerging therapies designed to address the specific characteristics revealed by ABSCINT-HER2.